Summary
Taking into account the angiographic characteristics of the treated lesions, as well as the treatment strategy, several significant differences were observed between the studied groups, while one independent risk factor for dissection was identified: the presence of at least moderate calcifications in the treated segment. The clinical complication rate observed in the 12-month follow-up was very low in the whole group, allowing for the conclusion that the occurrence of significant dissection can be effectively treated, and the good angiographic results of this treatment immediately after the initial procedure translate into good clinical results in longer, 1-year follow-up.
Introduction
Percutaneous coronary intervention (PCI) is a common, well-established method of treatment patients with coronary artery disease (CAD) and significant narrowing in coronary arteries. One of the most common complications during the PCI procedure is coronary artery dissection. The dissection could occur during the lesion preparation for stent implantation, and at this point in the procedure it is usually clinically not significant and could be treated successfully by stent implantation. However, if this kind of complication occurs after stent implantation, usually on the proximal or distal stent edge, it usually requires additional action to improve the result of the procedure and assure the patency of the treated vessel. Usually, a prolonged balloon inflation is sufficient, but sometimes the additional stent implantation is required, especially for the treatment of higher-grade dissections. There are several factors identified that are connected with higher risk of dissection during the PCI procedure, such as high-pressure inflations, calcifications in the target lesion, or overestimation of the device size.
Aim
The aim of the present publication is to describe the occurrence of coronary artery dissection after bioresorbable vascular scaffold (BVS) implantation, which is observed in angiography directly after scaffold implantation. This selected type of PCI procedure is especially interesting because precise target vessel measurement before BVS implantation is required for optimal determination of the scaffold size. What is more, high-pressure inflation, especially for post-dilatation is not recommended, so the factors increasing the risk of dissection during PCI procedure with BVS implantation could be different from those encountered during metallic stent implantation.
Based on angiographic data gathered in the POLAR ACS Registry, we assessed the frequency of dissections, and their localization and severity. Based on data regarding patient demographics, clinical status, and details regarding treatment strategy, the factors that could have an influence on the dissection occurrence were identified.
Material and methods
Study material
Data regarding the strategy and results of BVS implantation were gathered from the Polish Registry of patients with ACS treated by BVS implantation (POLAR ACS). The POLAR ACS Registry was compiled in 12 Invasive Cardiology Centres from November 2012 to September 2013. POLAR ACS was a one-arm prospective observational registry study, with an independent CoreLab employed for the angiography analysis (KCRI, Krakow, Poland).
A detailed description of patient demographics, clinical data, as well as QCA analysis was described in a previous publication [1].
Statistical analysis
The analysis was performed based on standard descriptive statistics. Categorical variables were presented as percentages. Continuous variables were expressed as mean with standard deviation or median (interquartile range). Differences between groups were compared using Student’s or Welch’s t-test, depending on the equality of variance for normally distributed variables. The Mann-Whitney U test was used for non-normally distributed continuous variables or for ordinal variables. Categorical variables were compared by Pearson’s χ2 test or by Fisher’s exact test.
All statistical analysis were performed using JMP®, Version 13.1.0., SAS Institute Inc., 2016. A p-value < 0.05 was considered as statistically significant.
Results
In total 100 patients were included in the analyses. This group was divided into 2 subgroups: Group A – dissection group, with patients in whom dissection was observed in angiography, and Group B – no-dissection group, without significant dissection observed in QCA after BVS implantation.
Group A consisted of 9 patients (9%, 9 lesions). This group was defined as patients in whom significant dissection occurred after BVS implantation. Dissection was considered ‘significant’ when, according to the operator, it required an additional action to treat this complication. This intervention was in most cases an additional stent implantation (8 patients; in 4 patients one additional BVS, in 1 patient 2 additional BVS; in 3 patients one additional metallic stent) and prolonged inflation of balloon catheter (1 patient). Group B comprised 91 patients (92 lesions).
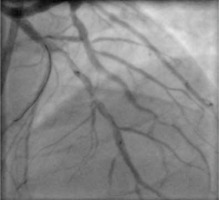
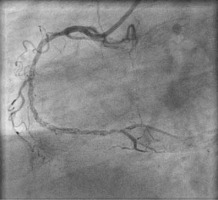
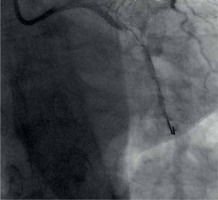
Dissection after predilatation, before BVS implantation, occurred in 22 patients, and in 17 of them it was covered by BVS implantation with optimal angiographic results. Five of them were finally in the dissection group. In another 4 patients from the dissection group, dissection appeared after BVS implantation and required additional intervention, but it was absent after predilatation. The description of dissection according to the NHLBI classification [2] is presented in Table I. Examples of angiographic images of individual dissection classes are shown in Table II.
Table I
Demographic and medical characteristic of the study groups
Table II
Coronary artery dissection – classification
Both groups are very similar according to demographic data (Table I). More than one stent was often implanted in the dissection group as a consequence of group definition.
The treatment strategy in both study groups was similar. The frequency of predilatation was similar; post-dilatation was performed more often in group A but without statistical significance. The balloon catheter for predilatation as well as for post-dilatation was shorter than the implanted BVS (Table III).
Table III
Invasive treatment strategy – predilatation and BVS implantation
In Group B the predilatation (p = 0.0434; Table III), stent implantation (p = NS; Table III), and post-dilatation (p = 0.0444; Table IV) were performed with lower pressure than in group A.
Table IV
Invasive treatment strategy – post-dilatation details
At baseline, the length of the treated lesion was similar in both groups (p = NS; Table III). Pre-dilatation in Group B was performed with a longer balloon catheter, which had a smaller diameter than in Group A. The difference in balloon catheter length used for second predilatation was statistically significant (p = 0.0464; Table V). Nominal logistic regression indicated the presence of calcification in the target lesion as an independent factor of dissection during the index PCI procedure (OR = 1.2–42.7; p = 0.0325).
Table V
Invasive treatment strategy – predilatation details
Detailed analysis of pre-dilatation and post-dilatation strategy leads to the conclusion that in Group B, without significant dissection, the diameter of balloon catheters was less than in Group A, but post dilatation the diameter of balloon catheters was higher in Group B. These differences were without statistical significance.
The clinical complication rate observed in 12-month follow-up was very low in the whole group; it was one stent thrombosis with myocardial infarction and target vessel revascularization and one non-target vessel revascularization. Both events occurred in group B, without significant dissection during the initial procedure.
Discussion and conclusions
Dissection during the PCI procedure with BVS implantation, which required additional stent implantation, occurred in 9% of the study population. Patients with clinically significant dissection had a demographic and medical profile similar to the patients without this complication. Predilatation in patients with clinically significant dissection was performed with shorter balloon catheters but with higher inflation pressure; BVS implantation and post-dilatation were performed with higher inflation pressure than in patients without significant dissection. The presence of at least moderate calcifications in the treated segment turned out to be an independent risk factor for significant dissection.
Calcifications, as well as the suboptimal selection of the balloon catheter diameter, the presence of other lesions in the treated artery, and the lesion length, have been identified as dissection risk factors during percutaneous coronary angioplasty procedures [3]. The above-mentioned risk factors in most cases were quite effectively eliminated by selecting lesions in the coronary arteries that can be optimally treated with BVS implantation, as well as by paying special attention to the precise dimensioning of the treated lesion, and selection of the size of the stent and balloon catheter for predilatation. The obtained results suggest that the angiographic assessment often underestimates the presence of calcifications, which is confirmed by studies using intravascular imaging techniques, in which the percentage of calcification in the general population of patients undergoing invasive cardiology procedures reaches as much as 75% [4].
The published frequency of dissections after BVS implantation depends on the method of visualization; in OCT it is reported at up to 40% of lesion [5], while in angiographic assessment it is usually less than 10% [4].
In previous publications, post-dilatation of bioresorbable scaffolds was assessed as a safe procedure, which significantly improved the scaffold apposition without inducing higher rates of edge dissection or strut fracture [6]. The presented data confirm the safety of post-dilatation because in more than 66% of patients with significant dissection, dissection appeared at an early stage of the procedure, after predilatation.
The clinical complication rate observed in 12-month follow-up was very low in the whole group; 2 re-PCIs occurred in patients without significant dissection during the initial procedure. There was no association between dissections and MACE occurrence in the long-term follow-up. This observation is consistent with a previous report in which the 12-month major adverse cardiac event rate was similar between patients with and without dissections [7–10]. The results of 1-year follow-up allow for the conclusion that the occurrence of significant dissection can be effectively treated, and the good angiographic results of this treatment immediately after the initial procedure translates into good clinical results in longer, 1-year follow-up.
The presented study has several limitations; one of them being the relatively small group of patients. Moreover, the diagnosis of dissection was based only on the analysis of the angiographic image of the vessel, and no intravascular imaging was performed.