Summary
Electrocardiographic recordings that suggest high-risk anatomy, such as Wellens syndrome, de Winter sign, and ST-segment depression by ≥ 1 mm in ≥ 6 classic ECG leads accompanied by ST-segment elevation in aVR and/or V1 in patients with acute coronary syndromes, due to presumed general unawareness in the medical community, when unrecognized, can lead to undertreatment while being relatively frequent (29.69%) in patients with non-ST-segment elevation acute coronary syndrome and culprit lesions in left main coronary artery or left anterior descending artery. Early recognition of these patterns is of clinical importance and could be considered a valuable tool in identifying the need for significantly accelerated invasive strategy. Implementation of earlier cardiac catheterization in this group could potentially offer a more appropriate therapy selection. Further research is necessary to validate our preliminary observations.
Introduction
Acute coronary syndromes (ACS) are divided into two categories: ACS with persistent elevation of the ST segment (ST-ACS, i.e. with the presence of Pardee wave); and ACS without such elevation (NSTE-ACS), which is essential for determining the patient’s management. In the case of ST-ACS, the standard treatment involves reperfusion performed as soon as possible (up to 1.5–2 h), while patients with NSTE-ACS are subject to risk stratification, which determines the urgency of performing coronary angiography and, if necessary, coronary revascularization. According to the onset of symptoms and assessment during the initial medical contact with the patient, the therapeutic path can follow an immediate invasive (< 2 h), early invasive (< 24 h), or selective invasive strategy [1].
In the 2020 update of the European Society of Cardiology Guidelines for the management of NSTE-ACS [1], it was noted that in such patients, certain electrocardiographic recordings may indicate high-risk anatomy, i.e. critical stenosis or occlusion of the trunk or the proximal and/or middle segment of left anterior descending artery, despite the lack of Pardee wave in the ECG, which indicates a remarkable acceleration of the invasive strategy [1]. According to ESC guidelines, obtaining an electrocardiographic recording is recommended within 10 min of the initial medical contact for patients with ACS, and the analysis of the ECG is crucial in the decision-making process.
The above clinical situations include [1–11]:
– Wellens’ syndrome, i.e. 2-phase (positive-negative) T waves in leads V2-V3 (type A) or deep negative symmetrical T waves in leads V2-V3 (or V1-V6) (type B) in the absence of significant elevation of the J point (< 1 mm),
– de Winter sign, i.e. a 1–3 mm upsloping ST-segment depression at the J point in leads V1 to V6, turning into tall, positive symmetrical T waves,
– ST segment depression by ≥ 1 mm in ≥ 6 classic ECG leads with simultaneous ST segment elevation in leads aVR and/or V1.
There is a relative paucity of reports regarding clinical characteristics of large series of high-risk ECG patients. Therefore, our objective was to summarize the features of the mentioned subgroups, along with an additional analysis of the frequency and potential factors that could increase the likelihood of the presented phenomenon occurring.
Aim
The aim of our study was to estimate the frequency of the observed phenomenon, i.e. ECG patterns suggestive of high-risk coronary anatomy recognized as indications for an urgent invasive approach in non-ST-segment elevation acute coronary syndromes (NSTE-ACS). Additionally, our research aimed to assess clinical characteristics of NSTE-ACS subjects associated with Wellens syndrome, de Winter sign, or ST-segment depressions by ≥ 1 mm in ≥ 6 classic ECG leads with simultaneous ST-segment elevation in aVR and/or V1.
Material and methods
Patients
Out of 207 subjects previously hospitalized in the Second Department of Cardiology and Cardiovascular Interventions at the University Hospital in Krakow and Clinical Department of Interventional Cardiology at John Paul II Hospital in Krakow between 2021 and 2023, with a final diagnosis of NSTE-ACS (unstable angina (76), or no ST segment elevation myocardial infarction (131)), 64 subjects who met the inclusion criteria and had available documentation of their admission electrocardiogram and performed coronary angiography during the hospitalization entered the final analysis (26 women and 38 men). The applied exclusion criteria, which narrowed down the final set of analysed cases, included lesions limited to the right coronary artery (RCA), non-significant (≤ 40%) lesions in the left coronary artery, and incomplete medical records.
Data analysis
Medical records of 207 subjects diagnosed with NSTE-ACS were retrospectively collected from the clinics’ archives. After applying exclusion criteria, which encompassed incomplete medical documentation, lesions limited to the RCA, and non-significant (≤ 40%) stenosis of the LCA, 64 out of 207 patients with complete medical records including admission electrocardiogram, who underwent coronary angiography during the index hospitalization, and presence of significant culprit stenosis or occlusion of the left main coronary artery or proximal/middle segment of the left anterior descending artery entered the final analysis.
Cases were divided into 2 subgroups based on the characteristic ECG patterns. Patients representative of the high-risk ECG group (Wellens syndrome, de Winter sign, ST segment depression by ≥ 1 mm in ≥ 6 classic ECG leads with simultaneous ST segment elevation in leads aVR and/or V1) were identified and compared with their counterparts.
The study protocol was approved by the Jagiellonian University Bioethics Committee (no. 1072.6120.310.2021 dated 15/12/2021 with amendments approved on 23/02/2022 and 17/05/2023).
Statistical analysis
The data were described with use of standard descriptive statistics. Categorical variables are presented as percentages and were compared using Pearson’s c2 test. Continuous variables are displayed as mean values and standard deviations (SD) for normally distributed data, and as medians with interquartile range (Q1-Q3) for non-normally distributed data. The Shapiro-Wilk test was used to assess the data normality. Quantitative variables with a normal distribution were compared using Student’s t-test for 2 groups. Non-normally distributed quantitative variables were compared using the Mann-Whitney-Wilcoxon U test for 2 groups.
The level of statistical significance was assumed set at a p-value of < 0.05. All analyses were conducted using TIBCO Statistica software (version 13. Palo Alto, CA, USA).
Results
Patients’ characteristics
Out of 64 subjects, who, on the basis of exclusion criteria, entered the final analysis, high-risk electrocardiographic patterns, including Wellens syndrome, de Winter sign, and ST segment depressions, were present in 19 cases (29.69%; 8 men, 11 women with a median age of 69 years [Q1–Q3: 63.5–74.5]): 10 (15.63%), 0 (0%), and 9 (14.06%), respectively. The patients’ characteristics were compared with their 45 counterparts (30 men and 15 women with a median age of 69 years [Q1–Q3: 65–77]). Table I describes the occurrence of lesions in specific locations, divided by the corresponding high-risk ECG recordings.
Table I
Occurrence of lesions in the left coronary artery divided by high-risk ECG patterns (Wellens’ syndrome, de Winter syndrome, ST segment depression by ≥ 1 mm in ≥ 6 classic ECG leads with simultaneous ST segment elevation in leads aVR and/or V1)
The aspect of crucial importance in our study was to assess the clinical characteristics of patients presenting with high-risk ECG in comparison to their counterparts. There were no significant intergroup differences in most of the patients’ characteristics concerning collected data, which included hypertension, diabetes, and previous medical history (myocardial infarction, percutaneous coronary intervention, coronary artery bypass grafting). The only statistically significant difference between the groups pertained to a positive interview regarding nicotinism (p-value: 0.044). In the high-risk ECG group, this percentage was 47%, while in the non-high-risk ECG group it was 22%. The results of the comparison of clinical characteristics between the subgroups are presented in Figure 1 and Table II. Changes observed during urgent angiography of the left coronary artery in patients with (1) Wellens syndrome or (2) ST-segment depressions by ≥ 1 mm in ≥ 6 classic ECG leads with simultaneous ST-segment elevation in aVR and/or V1 are presented in Figure 2.
Table II
Comparison of selected features in patients with and without ECG patterns suggestive of high-risk coronary anatomy in non-ST-segment elevation acute coronary syndromes, presenting critical stenosis or occlusion of LMCA or proximal/middle LAD
Figure 1
Comparison of clinical characteristics between patients with and without ECG patterns suggestive of high-risk coronary anatomy in non-ST-segment elevation acute coronary syndromes, presenting critical stenosis or occlusion of LMCA or proximal/middle LAD
CABG – coronary artery bypass grafting, CAD – coronary artery disease, MI – myocardial infarction, NSTEMI – no ST-segment elevation myocardial infarction, PAOD – peripheral arterial occlusive disease, PCI – percutaneous coronary intervention, UA – unstable angina.
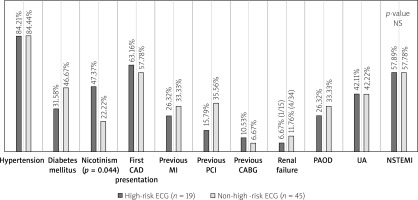
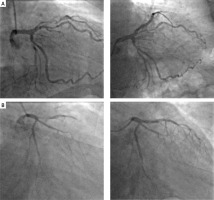
Figure 2
Urgent angiography of the left coronary artery: A – Wellens syndrome; proximal LAD lesion (left: pre-PCI, right: post- PCI); B – ST-segment depressions by ≥ 1 mm in ≥ 6 classic ECG leads with simultaneous ST-segment elevation in aVR and/or V1; ostial LAD lesion (left: pre-PCI, right: post- PCI)
Discussion
In our analysis, we aimed to identify the frequency and clinical characteristics of patients representing high-risk coronary anatomy in NSTE-ACSs, particularly critical stenosis or occlusion of LMCA or proximal/middle segment of the left anterior descending artery (LAD). We provided a separate discussion regarding each of the mentioned electrocardiographic recordings (i.e. Wellens syndrome, de Winter sign, ST segment depression by ≥ 1 mm in ≥ 6 classic ECG leads with simultaneous ST segment elevation in leads aVR and/or V1), because since Supplementary Figure 3 presented in the 2020 ESC Guidelines for the managements of NSTE-ACS [1], regards them jointly as significant in recognizing STEMI-equivalent patterns, indicative of high-risk coronary anatomy.
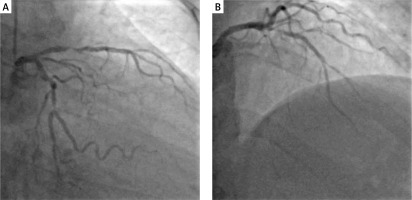
Figure 3
Critical high-grade stenosis within the middle segment of the left anterior descending artery in a patient with an admission ECG recording showing ST-segment depressions (by 0.5 mm) in ≥ 6 classic ECG leads and ST-segment elevation (0.5 mm) in the aVR lead (pre-PCI)
According to the 2020 ESC Guidelines for the management of NSTE-ACS [1], patients with ECG ST-segment depression ≥ 1 mm in ≥ 6 classic ECG leads with simultaneous ST segment elevation in leads aVR and/or V1 belong to a very high-risk category and should undergo an immediate invasive strategy (< 2 h), which is widely recognized among practicing physicians. In an earlier study from 2001, Yamaji et al. reported that ST segment elevation in lead aVR with less ST segment elevation in lead V1 is notably significant in predicting acute LMCA obstruction [2]. They reported that when encountering cases of acute LMCA obstruction, the elevation of the ST segment in aVR could play a part in predicting the patient’s clinical outcome. Conversely, in 2007 Yan et al. assessed the correlation of ST elevation in lead aVR with angiographic findings and outcome in NSTE-ACS. They observed that while ST elevation in aVR is linked to increased rates of unadjusted in-hospital and 6-month mortality, it does not present additional predictive benefit beyond a thorough risk assessment using the established GRACE risk model. Nonetheless, ST elevation exceeding 1 mm in aVR holds potential for promptly detecting left main or triple vessel disease in ACS patients who also exhibit ST segment depression [3].
Our study suggests that both critical stenosis (> 40–99%) and occlusion of LMCA or proximal/middle segment LAD should be recognized as relatively frequent in cases of ST segment depression ≥ 1 mm in ≥ 6 classic ECG leads with simultaneous ST segment elevation in leads aVR and/or V1. However, it should be noted that our study does not provide analysis of counterpart data, i.e. subjects’ subgroup with mentioned high-risk ECG patterns and a lack of significant lesions in the left coronary artery, which marks our conclusions as preliminary.
Previous studies reveal that ST-elevation in lead aVR is not solely connected to the ST-segment depression pattern. According to De Winter et al., in most of the cases positive for the next analysed high-risk pattern, i.e. de Winter sign, there was also a 1- to 2-mm ST elevation in lead aVR [4]. In 2008, they explored the correlation between ECG performed on the initial medical contact with the patient and the coronary angiogram. They described a new ECG pattern without ST-segment elevation, which signifies occlusion of the proximal LAD. They noted that as opposed to the characteristic ST-segment elevation, the ST segment exhibited a 1- to 3-mm upsloping ST-segment depression at the J point in leads V1 to V6, which continued into tall, positive symmetrical T waves present in 2.0% (30/1532) of patients with anterior myocardial infarction [4], later named de Winter sign. In our analysis, the mentioned pattern was not present in any of the patients admitted due to lesions in the LCA, which we attribute to the low number of examined patients.
The significance of de Winter pattern is highlighted in Lu et al.’s case report, which also mentions its in-time evolution, suggesting that de Winter syndrome might represent a temporary change in the course of ACS, potentially evolving into a conventional STEMI-pattern ECG or even normalizing [5, 12]. Hence, the documented instance implies that unless the ECG is promptly monitored, the characteristic ECG alterations seen in de Winter pattern might go unnoticed. Even if the ECG shifts to a typical STEMI-pattern, a clinical progression to STEMI is not observed [5].
In 2002, Rhinehardt et al. noted that following the definitive treatment of stenosis in the proximal LAD artery, the electrocardiographic pattern known as Wellens’ syndrome, characterized by T-wave alterations accompanied by a record of anginal chest pain without serum markers irregularities, resolves concurrently with the return of the electrocardiogram to a normal state. In the absence of intervention, the T-wave abnormalities remain present and can persist for hours to weeks. These changes are often observed by medical practitioners in asymptomatic patients [6].
Due to limitations in medical recordings, we aimed to focus on ECG abnormalities; however, the correlation between the pain-free state and ECG patterns is an important target for further investigation. In 2008, Movahed MR reported that the existing literature employed 2 different terms: Wellens’ syndrome or inverted U-waves, to name the same ECG pattern. Frequently, authors utilized either one of these terms, indicating a widespread lack of recognition within the medical field concerning this specific electrocardiographic phenomenon [7].
Clinical features of “STEMI equivalents” have been widely described; however, an overview of patient characteristics was not recognized. According to our study, no significant clinical differences between the presented subgroups were identified, which remains in line with De Winter et al. [4], who did not determine distinct patients’ characteristics (nor angiogram) that conclusively differentiated the de Winter pattern from a pattern of anterior ST-segment elevation.
Presented patterns, with inclusion of ‘grey-zone cases’, where the mentioned ECG patterns are not prominent, but which also correspond with critical stenosis or occlusion of LMCA or proximal/middle segment of LAD, appear to be relatively frequent (29.69%) and are subject to PCI and further treatment. To recognize the importance of grey-zone cases, we would like to introduce a case of a female patient with a 2-week history of crescendo angina. In the presence of clinical symptoms and an on-admission ECG recording showing ST-segment depressions (by 0.5 mm) in ≥ 6 classic ECG leads and ST-segment elevation (0.5 mm) in the aVR lead, routine use of hs-cTn (result: 94 ng/l) was ordered to establish the appropriate diagnostic algorithm. A performed urgent coronary angiography revealed 99% stenosis of the proximal segment of the left anterior descending artery (Figure 3).
The results of our study, by showing no significant intergroup differences, revealed the presumed importance of identifying high-risk electrocardiographic recordings as specific for an accelerated invasive strategy, despite the lack of a classic Pardee wave in the ECG. Based on the collected data, we believe that recognizing the mentioned patterns may prove useful in identifying high-risk patients who require a notably accelerated invasive strategy in NSTE-ACS cases.
Conclusions
The mentioned electrocardiographic recordings that suggest high-risk anatomy, such as Wellens’ syndrome, de Winter sign, and ST-segment depression by ≥ 1 mm in ≥ 6 classic ECG leads accompanied by ST-segment elevation in aVR and/or V1 in patients with acute coronary syndromes, due to presumed general unawareness in the medical community, when unrecognized, can lead to undertreatment while being relatively frequent (29.69%) in patients with NSTE-ACS and culprit lesions in LMCA or LAD. Early recognition of these patterns is of clinical importance and could be considered a valuable tool in identifying the need for a significantly accelerated invasive strategy. Implementation of earlier cardiac catheterization in this group potentially offers a more appropriate therapy selection. Further research is necessary to validate our preliminary observations.








