Inflammatory linear verrucous epidermal nevus (ILVEN) is a rare, pruritic, erythematous, scaly epidermal nevus that spreads along the Blaschko’s lines. It is usually located unilaterally on the left lower extremity, has an early age of onset, and is predominant in females [1]. However, several atypical cases of ILVEN, such as familial occurrence and adult onset [2], generalized [3], or giant lesions [4], have been reported. So far, various therapeutic approaches have been described, including the use of topical agents [5–7], systemic medications [8, 9], physical modalities [10, 11], and surgical excision [4, 12]. Because the predominance of any of the methods have not been proven, the treatment choice should depend on the patient’s age, location and the size of the lesions.
This report presents the case of a 69-year-old man who was admitted to our dermatology department for examination of a giant linear tumour on his left lower extremity. He had a history of hypertension, diabetes mellitus, mixed hyperlipidaemia, atrial fibrillation and flutter, atherosclerotic cardiovascular disease, varicose veins of lower extremities, cerebral infarction in the past, and he was on numerous medications due to above-mentioned conditions.
Clinical examination revealed a brown, verrucous, hyperkeratotic tumour on the dorsum of the left foot extending to the lateral ankle and posterior surface of the lower leg. Erythematous papules were present above the tumour, which formed along the Blaschko’s lines reaching from the left popliteal fossa, through the posterior surface of the thigh, and to the left buttock (Figures 1 A, C). The patient reported that erythematous lesions in the left popliteal fossa with mild pruritus had been present and stable in this form since his childhood. However, for the last 2 years, the patient had noticed the expansion of the verrucous lesion on the lower leg, but he denied the presence of pruritus. Family history was negative for any dermatological disorders.
Figure 1
Inflammatory linear verrucous epidermal nevus (ILVEN) on lower left extremity: posterior surface before (A) and after (B) surgical treatment and cryosurgery; dorsum of the foot and lateral ankle before (C) and after (D) surgical treatment and 0.5% 5-FU with 10% salicylic acid solution applications

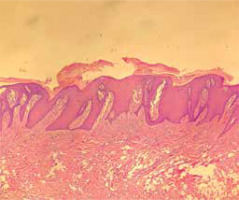
According to the clinical presentation, the differential diagnosis included ILVEN and carcinoma cuniculatum. To conduct a histological examination, samples of tissue of the lesions from the lateral ankle and the gluteal region were taken. Histology showed thickening of the epidermis, hyperkeratosis with alternate parakeratosis, acanthosis, and perivascular inflammatory infiltrates in the dermis (Figure 2). Based on clinical and histopathological findings, the patient was diagnosed with a giant ILVEN. Because of the giant size of the patient’s lesions, we decided to deploy a combined treatment. Initially, the patient had undergone simple surgical excision and closure of the plaques below the gluteal region followed by resection of the tumour on the dorsum of the left foot after 5 months (Figures 1 A–D). The postoperative period was uneventful, and no recurrence was observed.
Figure 2
Histopathology showing thickening of the epidermis, hyperkeratosis with alternate parakeratosis, acanthosis, and perivascular inflammatory infiltrates in the dermis (H and E, 40 × magnification)
Subsequently, due to the patient’s serious cardiovascular diseases, we decided to implement cryosurgery as the method of treatment, which was applied to the tumour on the posterior surface of the lower leg. During the procedures, the nozzle of the cryogun spray was held 1 cm from the lesion throughout the freezing. Deep freezing was continued until the moment that it required approximately 1 min thawing time without repeating. The treatment by cryodestruction has been executed once a month in 8 stages until now. Additionally, the patient was instructed to apply a solution containing 0.5% 5-FU and 10% salicylic acid twice a day on 2 selected areas: the lesions above and below the lateral ankle.
In the 12-month follow-up period since the first excision, no recurrences have been found in the surgically treated areas. The hyperkeratotic component of the lesion undergoes monthly cryosurgery treatment; however, the lesion extends. The areas treated with 5-FU and salicylic acid also progressed (Figures 1 C, D). The treatment has been well-tolerated – so far, no clinically important side effects or complications have developed.
Inflammatory linear verrucous epidermal nevus was first described by Altman and Mehregan in 1971 [1]. They suggested that ILVEN tends to be highly resistant to any form of treatment. Differential diagnosis of ILVEN includes linear psoriasis, lichen striatus, linear Darier disease, linear porokeratosis, linear lichen planus, and carcinoma cuniculatum [4]. To date, no single ILVEN therapy has been proven to be effective in most patients. In reviewing the literature, the descriptions of successful treatment with tacrolimus [5], topical steroids [6], and 5-FU [7] were found. In the cases of large ILVEN lesions resistant to topical treatment, studies showed promising results of systemic treatment with oral acitretin [3] and anti-TNF antibodies such as etanercept [8] and adalimumab [9]. Other studies presented successful treatment with a 308-nm excimer laser [10] and carbon dioxide laser [11]. Surgical treatment is presented most frequently in cases of giant and extensive lesions [4, 12].
Cryosurgery seems to be one of the methods used less frequently in the treatment of ILVEN. This surgical technique consists of freezing to achieve the destruction of tissue. The mechanism of damage is complex and involves intracellular ice crystal formation, electrolyte concentration, thrombosis and stasis in vessels, and inflammation through immunological response after freezing [13]. Only a few studies concerning the treatment of ILVEN with cryotherapy have been published. In 1983, Fox and Lapins [14] examined the efficacy of numerous methods or treatment of a disfiguring, extensive ILVEN in the case of a teenage girl. Cryotherapy using liquid nitrogen proved to be the most successful, and it was used to treat almost all this patient’s lesions with good cosmetic results. This study also presented some positive results of using topical 5-FU, but the effects were less effective than cryosurgery. In a different study, Lapidoth et al. [15] presented the results of cryosurgery of 71 patients with verrucous epidermal nevus (VEN). Treatment results of patients with ILVEN were variable: 2 patients achieved 75–100% lesion clearance, 2 patients achieved 25–50% lesion clearance, and 2 patients achieved < 25% lesion clearance. Partial recurrence, 13 and 16 months after the end of treatment, was noted in 2 of the 4 patients, with fair to excellent response.
Our patient has been treated with cryosurgery, surgical excision, and 0.5% 5-FU with 10% salicylic acid solution. Although treatment efficacy with 5-FU [7] and cryosurgery [15] has been reported in the literature, the satisfactory effect in our case is observed only in the surgically treated areas.
In conclusion, there is no single therapy that has been found to be effective in all cases. Depending on size, localization of lesions, and the age and general condition of the patient, different methods of treatment may be considered. The most successful method in our case of giant ILVEN was surgical excision.








