Introduction
Acne belongs to the most common dermatoses [1]. Acne lesions are common in adolescents, however, they may also appear in adults. The worldwide prevalence of acne among adolescents is assessed as 80% and among adults as 40% [2, 3]. Acne with the visibility of lesions, predominantly located on the face, has severe psychosocial consequences [4–6]. Acne may also be classified as a psychophysiological disorder, which is exacerbated by psychological stress [7]. It is obvious that the military conflict in Ukraine is experienced by people as acute and chronic stress [8]. Several dermatological diseases, including chronic inflammatory ones like psoriasis, have been reported to be exacerbated during the war [9].
Aim
This study was undertaken to evaluate the severity of acne in patients seeking dermatological treatment during the military conflict in Ukraine. Special attention was put to patients’ opinions on the exacerbation of acne during the period of war activities.
Material and methods
Subjects
The studied group consisted of 143 consecutive patients with acne from the region of Dnipro, Ukraine, visiting dermatology units for acne treatment. There were 90 (62.9%) females and 53 (37.1%) males with a mean age of 21.24 ±6.37 years (range: 11–43 years). The majority of them – 135 (94.4%) were civilians, and the remaining ones – 8 (5.6%) patients, all males, served in the army. The duration of acne ranged between 2 months and 24 years, with a mean value of 4.13 ±3.89 years.
Diagnosis and assessments
Acne vulgaris was diagnosed by a dermatologist based on anamnesis and clinical manifestation. The severity of acne was assessed with Investigator’s Global Assessment (IGA). This is a validated tool that grades acne from 0 points (clear skin) to 4 points (severe acne) [10]. Moreover, all patients were asked for the presence of itch within acne lesions during the whole period of disease and during the last 3 days. The intensity of the worst itch during the last 3 days was evaluated with the Numeral Rating Scale (WI-NRS) [11]. The intensity of itch was based on the following cut-off points of NRS: 0 points – no itch, 1–3 points – mild itch, 4–6 points – moderate itch, 7–8 points – severe itch, and at least 9 points – very severe itch [11]. Patients also expressed their personal opinion on the exacerbation of acne during the military conflict based on the simple question: “Have you observed an exacerbation of acne during the war?”. A similar question was asked on the flare of the itch “Have you experienced an exacerbation of itch within acne lesions during the war?”. The study was conducted according to the Declaration of Helsinki with the Ethical Committee approval of Wroclaw Medical University (No. KB-234/2023).
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics v. 26 (SPSS INC., Chicago, IL, USA) software. In the beginning, all the data were assessed for parametric and non-parametric distribution using the Kolmogorov–Smirnov normality test. The minimum, maximum, mean, standard deviations and ranges were calculated. The Student’s t test or Mann-Whitney U test for parametric and non-parametric data were employed for quantitative data. Depending on normality, Spearman’s and Pearson’s correlations were used for the correlation assessments. Qualitative data were analyzed using the χ2 test. A 2-sided p-value less than 0.05 was statistically significant.
Results
The mean severity of acne assessed with IGA was 2.27 ±0.81 points. Twenty-five (17.5%) patients presented with very mild acne, and 55 (38.5%) patients with mild acne. Fifty-six (39.2%) subjects were diagnosed with moderate acne, and the remaining 7 (4.8%) patients with severe acne. There was no difference in acne severity between female and male patients (Table 1). Itch within acne lesions during the whole disease period was reported by 25 (17.4%) patients, and it was present in 13 (9.1%) patients during the last 3 days. The mean itch intensity assessed with WI-NRS was calculated as 3.94 ±2.91 points. The clinical acne severity did not correlate with the duration of acne and with the itch intensity (detailed data not shown). Seventy (50.7%) out of 138 patients declared the exacerbation of their acne during the military conflict. Five (3.5%) patients of the whole studied group (143 acne patients) did not provide an answer to this question. There was no difference in gender concerning self-assessment of acne lesions due to war activities (Table 2). Acne itch exacerbation during the war was reported by only 9 (36.0%) out of 25 itchy subjects.
Discussion
Acne is a chronic inflammatory skin disease. Acne course seems to be unpredictable, but in many patients, acne lasts for many years, even more than 10 years. The majority of acne subjects present with rather mild disease, severe and very severe acne is diagnosed in about 20% of patients [1, 2]. Acne, although not a life-threatening condition, should not be considered only a cosmetic problem. Acne was demonstrated to have a vast influence on the psychological status of patients [4–6]. Most probably, this is due to the chronicity of the acne process, but also due to the location of acne lesions on visible skin areas, mainly the face. The face is treated as a predisposing location for acne; however the back and upper part of the chest are also commonly involved [1, 2].
Many studies demonstrated that acne predisposes to secondary psychiatric disturbances, like depression and anxiety [4, 12]. Also, patients with acne are at increased risk for suicidal thoughts and attempts [13]. Moreover, acne subjects have a markedly decreased quality of life (QoL) and are heavily stigmatized [5, 6]. The correlation between alexithymia, the ability to identify and verbally express emotions, and decreased QoL as well as an increased level of stigmatization was documented [14]. Itch within acne lesions seems to be a common phenomenon, and it can additionally contribute to the psychosocial burden of the disease [15].
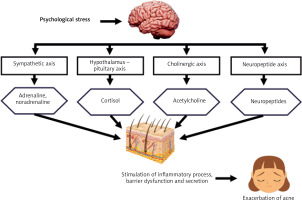
Having skin conditions, especially of chronic course and on visible skin areas, creates psychological stress for acne patients. Previous studies clearly showed that stress is a consequence of acne [16, 17]. However, psychoemotional stress may also cause or exacerbate acne lesions [16, 17]. It is well known that psychological stress may alter the immune system of the skin, directly affect sebaceous glands as well as may have an influence on the skin barrier [16, 17]. Psychoemotional stress is perceived by the central nervous system and results in activation of the hypothalamic-pituitary-adrenal (HPA) system leading to the release of numerous neuro mediators and activation of the autonomic nervous system at the periphery, including the skin. Subsequently, activated immune cells in the skin stimulate the pro-inflammatory process [16, 18]. Moreover, the release of corticotropin-releasing hormone, glucocorticoids, and adrenal androgens has been reported to be increased [19]. This leads to easier conversion of androgen precursors to testosterone and decreases the permeability of the skin, also increasing sebaceous hyperplasia. Stress also decreases antimicrobial resistance, which may have an essential role in the acceleration of acne lesions [16, 17]. Figure 1 presents the pathways of acne exacerbation by psychological stress. The relation between mind and skin is bilateral, and stress contributes to the vicious circle of acne pathogenesis, exacerbating acne and subsequently being the result of acne.
Analysing clinical studies on acne exacerbation due to psychoemotional stress, one may conclude that the literature on the above-mentioned topic is rather limited. However, in various studies of different designs, 50% to 82% of acne patients declared that psychological stress exacerbated their acne [17, 20–23]. Their correlation between stress and acne severity was also demonstrated [24]. Griesemer [25] documented that acne is usually exacerbated within 2 days after the stressful episode. It was also suggested that intense anger may cause acne flare. It is worth mentioning that stress was also reported as an important exacerbating factor of other chronic dermatoses [26]. The above-mentioned data are in agreement with our results, showing that more than 50% of acne patients reported their disease exacerbation due to war. Interestingly, only 36% of itchy subjects reported itch flare during this period. However, it is important to underline that itch was reported quite rarely in the studied group in comparison to the previous studies [15, 27, 28]. This may indicate that subjective sensation such as itch is not a crucial acne symptom during with the period of the military conflict. Recently, several authors have shown that the military conflict in Ukraine causes continuous traumatic stress to Ukrainian civilians [8, 29] as well as within civilian populations in different countries [30]. It is also obvious that soldiers are under huge stress during warfare operations. Our study group consisted mainly of the civilian population, with a very limited number of people directly involved in military activities. However, in the review by Gelman et al. [31] acne ranked fourth in the list of most common reasons for physician consultations for dermatological problems among soldiers during combined modern warfare and peacekeeping operations, including the Vietnam War, First Gulf War, Peacekeeping in Bosnia and East Timor, and Operation Iraqi Freedom.
We are aware of our study limitations. Firstly, the study was conducted only in one region of Ukraine. Secondly, it was based on self-reported data on the exacerbation of the disease. A prospective, multicentre study with the assessment of stress and acne flares by physicians should be conducted to confirm our results. On the other hand, the organization of such a study is almost impossible during the ongoing war activities. Based on the above-mentioned limitations, the results of the current study should be treated with caution.