The purported link between “chronic” coronary slow flow phenomenon (CSFP) and reduced flow across the microvasculature is increasingly challenged. When flow is measured in the presence of CSFP, either with doppler flow-wire or continuous-thermodilution, there is no demonstrable relationship between the two [1 2]. On the other hand, “acute” CSFP in the setting of atherosclerotic crud, clots, or air embolism is usually transient, presumably from microvascular obstruction or spasm [3]. This is usually dramatic, with chest pain and electrocardiographic changes, reminiscent of the very first accidental right coronary angiography in 1958 by F. Mason Sones in Cleveland Clinic. Therefore, the mechanism of “acute” CSFP may not be extrapolatable to “chronic” CSFP, especially because often patients with marked “chronic” CSFP seen on diagnostic coronary angiography are seemingly asymptomatic coming off the cardiac catheter laboratory table.
This brings us to the report by Figura et al. [4], for which there are 3 pertinent questions. First, with regards to the bolus-thermodilution, the variance of the resting mean transit times is nearly 50% (0.44 s to 0.87 s). Updated software would error-highlight a 30% discrepancy. Nevertheless, given the clear hyperaemic shortening of the transit times, the haemodynamic indices would be normal, suggesting an intact microvasculature. Second, as per the angiographic frame counts presented, the baseline flow was normal without CSFP. Which means that the response to 2 µg acetylcholine could be due to a “no reflow” phenomenon from inadvertent air embolism. For definitive diagnosis of acetylcholine-induced microvascular spasm, a rechallenge with the same dose or an escalated dose would remove any doubt. Third, the patient has exertional and not rest angina. In the absence of coronary microvascular dysfunction (CMD), the diagnosis of microvascular spasm does not sit well because it would be situational rather than exertional. Neither would this explain the angina with inferolateral ST-depression during the exercise test. The only other possibilities are arrhythmias, myocardial bridging, and anomalous origin of the coronary arteries. However, these are not evident from the data provided.
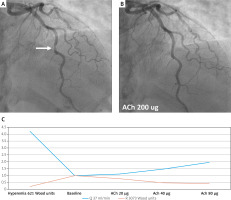
The emerging technique of continuous-thermodilution allows the absolute flow to be measured. CSFP due to acetylcholine-provoked microvascular spasm would be associated with flow reduction that could be estimated. Figure 1 shows a middle-aged postmenopausal woman who is an ex-smoker with diabetes, hypertension, hyperlipidaemia, polycystic ovary syndrome, and subclinical hypothyroidism. She has non-obstructive atherosclerotic plaques in the mid left anterior descending (LAD) artery and proximal right coronary artery (RCA). Both her central aortic blood pressure of 133/81 mm Hg and left ventricular end-diastolic pressure (LVEDP) of 12 (< 15) mm Hg are within normal limits. Acetylcholine causes LAD mild vasodilatation, indicating preserved endothelial function. This is confirmed on continuous-thermodilution in the RCA, which also finds intact vasodilatory capacity but raised coronary resistance. The latter is akin to elevated systemic vascular resistance due to chronic hypertension. This case illustrates the complexity of coronary haemodynamics. However, there could be 3-fold assessment for endothelial function, coronary resistance, and vasodilatory reserve. These allow tailored therapy, and the underlying aetiological factors could be targeted individually.
Figure 1
Coronary haemodynamics and continuous thermodilution. LAD before and after acetylcholine 200 μg without provokable vasospasm (A, B). Baseline low flow and high resistance in the RCA on continuous thermodilution, coronary flow and microvascular resistance reserves are normal at 4.2 and 4.9, respectively, flow increases > 1.5-fold with acetylcholine, and absolute microvascular resistance is 621 (< 500) Wood units, equivalent to an IMR of 31, which is high (fractional changes in flow and resistance from the nominal baseline of “1”, C)