Summary
Coronary computed tomographic angiography is an excellent diagnostic tool in evaluation of bifurcation lesions as it can accurately evaluate atherosclerotic plaques. In this study we found that the computed tomography (CT) bifurcation score was a very significant predictor of side branch occlusion during percutaneous coronary intervention. It had 80% sensitivity and 60% specificity at a cut-off point of 3. Direct comparison of the CT bifurcation score and corresponding angiographic scoring systems revealed that the CT bifurcation score outperformed both the Medina score and the Resolve score in prediction of side branch occlusion.
Introduction
Bifurcation lesions are prevalent as a result of atherosclerosis commonly occurring at branching areas [1]. About 15% to 20% of the bifurcation lesions are treated with percutaneous coronary interventions (PCI) [2].
They are difficult as they have a significantly reduced procedural rate of success and a higher complication rate [3]. The recommended approach is to implant one stent with temporary side branch (SB) wiring [4].
Nevertheless, 20% to 30% of instances following main-vessel (artery) stent implantation involved side-branch blockage [5]. It could be related to periprocedural myocardial infarction (MI) and rewiring failure following main-artery implantation of a stent; the lesion features related to side-branch blockage remain unknown. An approach using two stents might be used to treat high-risk bifurcation lesions, while other lesions would be managed using a straightforward one-stent strategy with transient SB wiring if the SB obstruction risk in bifurcation lesions could be categorized before PCI [6].
Coronary computed tomography angiography (CCTA) is a very accurate non-invasive imaging method for a thorough evaluation of plaques causing atherosclerosis, with excellent accuracy in diagnosis [7]. We attempted to detect possible indicators of SB obstruction in bifurcation lesions following main-artery stent installation.
Aim
We aimed to determine whether preprocedural CCTA may indicate intraprocedural SB blockage undergoing PCI of bifurcational lesions.
Material and methods
This retrospective observational study was conducted on 200 bifurcational lesions of 200 coronary artery disease patients of different ages and sex. All included cases were stentable, with a side branch of ≥ 2 mm in diameter, and elective PCI to the bifurcation lesion had to be performed within 3 months after CCTA. Cases were collected from tertiary cardiac centers in Egypt, including the Islamic Cardiac Center (Al-Azhar University), National Heart Institute (Specialized Institutes), Military Cardiac Centers (in Cairo), and Al-Helal Hospital in Sohag (HIO) from March 2021 to March 2023.
Exclusion criteria included MI prior to the PCI procedure, lesions located in the left main trunk, CTO in the main branch or side branch, presence of a previously implanted stent in the target lesion, inadequate CCTA data caused by the poor image quality, hemodynamically unstable status and the presence of a patent bypass graft to the target vessel.
All patients underwent two steps of angiography for coronary bifurcational lesion evaluation and classification:
A) CCTA:
CCTA was done to obtain the parameters of the CT bifurcation score and then to calculate it. These 6 parameters were selected from previous similar studies: four parameters of previous CT bifurcation score studies (e.g., Lee et al.) [8]: plaques in the SB, plaque with calcification in the main vessel (MV) proximal segment, necrotic plaques in the MV proximal or SB segment, MV to SB vascular area ratio more than 4.3; and 2 Parameters from Risk prEdiction of Side branch OccLusion in coronary bifurcation intervention (RESOLVE) score parameters which can be evaluated by CCTA: the length of the lesion in the SB, and the angle between the SB and the MV. Each parameter was assigned one point to create the CT bifurcation score, which ranges from 0 to 6. Also, measurement of the calcium score at the site of bifurcation was done.
To obtain the CT bifurcation score, in brief, using a 64-slice or 128-slice scanner (Aquilion, Toshiba, Canon, Siemens, or Philips), CT images were analyzed by imaging specialists supervised by a cardiologist or radiologist using a cardiovascular workstation (Vitrea and similar software). The bifurcation lesion was divided into six segments of interest which covered the proximal and distal 5 mm segments from the bifurcation confluence. The proximal and distal segments were divided into the branch side and contra-branch (opposite the branch) side, respectively. Plaque in the bifurcation confluence is assigned to the contra-branch ostial side segment. The SB segment was the 5 mm segment from the SB ostium (Figure 1 A).
Figure 1
A – Schematic illustration of bifurcation plaque analysis using CCTA, B – CT bifurcation score
CCTA – coronary computed tomographic angiography, MV – main vessel, SB – side branch, CT – computed tomographic.
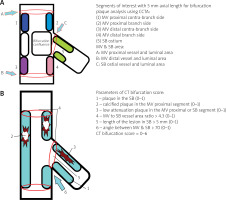
Quantitative assessments were carried out in each segment. The presence of plaque is defined by a diameter stenosis (DS) of ≥ 50% or an area stenosis of ≥ 75% within the segment of interest. The vessel and lumen areas are measured at the MV proximal or distal 5 mm from the bifurcation confluence and the SB ostium. Quantitative plaque volume of low attenuation, fatty, fibrous, and calcified plaque (defined by radiologic attenuation of –150–29, 30–149, 150–349, and 350–1,000 Hounsfield units (HU)) was assessed in each segment of interest (Figure 1 B).
As is customary in the RESOLVE score, the length of the lesion in the SB would be considered significant if it extended > 5 mm into the SB. Also, the angle between the MV and SB would be significant if it measured > 70°.
B) Coronary angiography and PCI:
Elective PCI was performed for patients who had significant stenosis on CCTA. The choice of treatment strategy and technique was at the discretion of the interventional cardiologist.
All of the following were evaluated: Intraprocedural SB occlusion was defined as the development of SB flows with Thrombolysis In Myocardial Infarction (TIMI) flow ≤ 1 after ballooning or stenting in the MV; quantitative coronary angiography (QCA) was performed by independent technicians. The reference diameter (RD), minimal luminal diameter (MLD), DS, and length were assessed in the proximal MV, the distal MV, the SB, and the bifurcation score segment, respectively, using the end-diastolic image; the bifurcation angle and the diameter ratio between the MV and SB were also assessed. Angiography-based bifurcations were classified using the Medina classification [9] and the RESOLVE (Risk prediction of side branch occlusion in coronary bifurcation intervention) score [10].
Ethical approval
The research was done after approval from the Ethical Committee at Al-Azhar University with approval number Car.-153.
Statistical analysis
The SPSS v26 statistical analysis program was used (IBM Inc., USA). Mean and standard deviation (SD) were used to display quantitative data. Frequency and percentages (%) were used to depict the qualitative variables. Spearman correlation was done to estimate the degree of correlation between two variables. Evaluation of diagnostic performance: diagnostic specificity and sensitivity, negative predictive value (NPV), positive predictive value (PPV), and receiver operating characteristic curve (ROC curve) analysis. A p-value < 0.05 is regarded as significant.
Results
Table I presents patient characteristics and clinical findings of the studied patients. The mean age was 57.78 ±7.33, and most of the studied cases were male (169, 84.5%).
Table I
Demographic and clinical finding of the studied cases (n = 200)
| Parameter | Value | |
|---|---|---|
| Age | Mean ± SD | 57.78 ±7.33 |
| Gender | Male | 169 (84.5%) |
| Female | 31 (15.5%) | |
| Ca score at bifurcational lesion | Mean ± SD | 20.68 ±19.63 |
| CT bifurcational score | Mean ± SD | 2.83 ±1.11 |
The Ca score at the bifurcational lesion had a mean of 20.68 ±19.63. The CT bifurcational score mean value was 2.83 ±1.11.
The parameters of the CT bifurcation score are shown in Table II. SB plaque was present in 86 (43%) cases. Calcified plaque in the MV was present in 134 (67%) cases, and necrotic plaque in the MV or SB was present in 146 (73%) cases. MV to SB vessel area ratio was > 4.3 in 53 (26.5%) cases. Length of the lesion in the SB was > 5 mm in 71 (35.5%) cases. The angle between the MV and SB was > 70° in 76 (38%) cases.
Table II
Parameters of CT bifurcation score of the studied cases
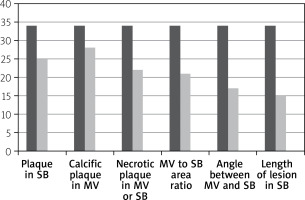
The distribution of CT bifurcation score parameters in cases with SB occlusion is shown in Figure 2. Plaque in the SB was present in 25 (74%) cases. Calcified plaque in the MV was present in 28 (82%) cases, and necrotic plaque in the MV or SB was present in 22 (64%) cases. MV to SB vessel area ratio was > 4.3 in 21 (62%) cases. Length of the lesion in the SB was > 5 mm in 17 (50%) cases. The angle between the MV and SB was > 70° in 15 (44%) cases.
Figure 2
CT bifurcation score parameters in cases with SB occlusion
MV – main vessel, SB – side branch.
Classification of SB occluded cases in the study according to the anatomical site was LAD – D in 29 instances, LCX – OM: (4) cases, and RCA – PDA: (1) case.
CT bifurcation score was: 0 in 3 (1.5%) cases, 1 in 12 (6.0%) cases, 2 in 69 (34.5%) cases, 3 in 63 (31.5%) cases, 4 in 42 (21.0%) cases, 5 in 7 (3.5%) cases, and 6 in 4 (2.0%) cases. The Medina score was: 1,1,1 in 56 (28%) cases, *0,1,1 in 19 (9.5%) cases, *1,0,1 in 8 (4%) cases, 1,1,0 in 37 (18.5%) cases, 1,0,0 in 34 (17%) cases, 0,1,0 in 43 (21.5%) cases, and 0,0,1 in 3 (1.5%) cases (*true bifurcational lesion presented in 83 (41.5%) cases). The RESOLVE score was: 0:4 in 44 (22.0%) cases, 4:7 in 43 (21.5%) cases, 8:11 in 58 (29.0%) cases, and 12 or more in 55 (27.5%) cases (Table III).
Table III
Relation between sex, CT bifurcation score, Medina score, and Resolve score and SB occlusion in the studied cases
There was no relationship between sex and SB occlusion in the studied cases. There was a significant relationship between CT bifurcation score and SB occlusion, significantly higher in patients with SB occlusion (p < 0.001). There was a borderline significant relation between Medina score and SB occlusion in the studied cases (p = 0.05). There was, unexpectedly, no relationship between the RESOLVE score and SB occlusion in the studied patients (Table III). There was a significant correlation between CT bifurcation score and both age and CA score (p < 0.001).
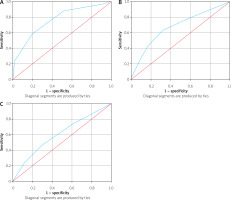
For the prediction of SB occlusion in bifurcational lesions during PCI, the CT bifurcation score can significantly detect SB occlusion (p < 0.001), with an AUC of 0.8 (95% CI: 0.67–0.89) and at a cut-off point of 3 showed 80% sensitivity and 60% specificity. The Medina score can borderline significantly detect SB occlusion (p = 0.05), with an AUC of 0.68 (95% CI: 0.58–0.74) with 60% sensitivity and 40% specificity. The RESOLVE score is an insignificant detector of SB occlusion (p = 0.25), with an AUC of 0.6 (95% CI: 0.5–0.7), with 40% sensitivity and 50% specificity (Figure 3).
Figure 3
ROC curve of CT bifurcation score (A), Medina score (B) and RESOLVE score (C) for detection of SB occlusion
ROC curve – receiver operating characteristic curve.
There were positive, highly significant correlations between the CT bifurcation score and both age (r = 0.5, p < 0.001) and Ca score (r = 0.6, p < 0.001).
Discussion
Bifurcation lesions represent about 15–20% of total lesions managed with PCI [11]. Bifurcation intervention SB occlusion constitutes a serious complication of the procedure that can have detrimental clinical results, such as clinically significant MI [12]. More recently, the use of CCTA has become widespread. This is certainly a result of enhanced scanning abilities, at least in part. The evaluation and risk classification of individuals who come with chest discomfort is now its primary purpose. While this is undoubtedly the most prevalent utilization of this technique, it may also be a useful complement in other contexts, including plaque evaluation, coronary artery stenosis functional evaluation, and complicated intervention planning [13].
The current study shows that the CT bifurcation score was significantly higher in patients with SB occlusion (p < 0.001). The present study can be supported by Lee et al. [8], who found that the CT bifurcation score was markedly higher in patients with SB occlusion (p < 0.001). They also found that the SB occlusion risk proportionally increased from 4.2% to 64.7% based on a CT bifurcation score of 0 to ≥ 3.
The current study shows a borderline significant relation between Medina score and SB occlusion in the studied cases (p = 0.05). The present study can be partially supported by Zhang et al. [14], Dou et al. 2015 [15], Hahn et al. [16], Grodecki et al. [17], and Opolski et al. [18], as all of these studies found a significant relation between Medina score and SB occlusion in the studied cases.
The current study shows that CT score can significantly detect SB occlusion (p < 0.001), with an AUC of 0.8 (95% CI: 0.67–0.89), and at a cut-off point of 3 showed 80% sensitivity and 60% specificity. The Medina score can significantly detect SB occlusion (p = 0.05) with an AUC of 0.68 (95% CI: 0.58–0.74) with 60% sensitivity and 40% specificity. The RESOLVE score is an insignificant detector of SB occlusion (p = 0.25) with an AUC of 0.6 (95% CI: 0.5–0.7) with 40% sensitivity and 50% specificity. The present study can be supported by Hennessey et al. [19], as they discovered that their CT bifurcation score included the existence of plaque within the SB, plaque that was calcified in the MV proximal segment, necrotic plaque in the SB segment or MV proximal, and an MV to SB vascular area ratio > 4.3, with a point allocated to each criterion. Cross-validation of the CT bifurcation score with both the RESOLVE score and the Medina classifications revealed that it outperformed both (c-statistic = 0.749 against 0.631 to 0.551; p < 0.05 for both). The CT bifurcation score’s accuracy, specificity, sensitivity, negative predictive value, and positive predictive value were 50%, 42%, 90%, 96%, and 23%, respectively.
Unexpectedly, the current study did not detect a relationship between the RESOLVE score and SB occlusion. Our results are inconsistent with Opolski et al. [18], who discovered that among 400 participants with 400 bifurcation lesions, there were 28 (7%) with SB obstruction, flow was absent in 12/28 (43%) of the lesions, but TIMI flow was reduced in 16/28 (57%) of them.
Also, our results are consistent with Lee et al. [8] in findings of both the CT bifurcation score and Medina classification, while being inconsistent with RESOLVE score findings of the same study, as they found that the risk of SB occlusion increased proportionally from 4.2% to 64.7% according to a CT bifurcation score of 0 to ≥ 3, whereas it increased moderately from 8.6% to 22.9% according to RESOLVE score quartiles, and from 0% to 26.4% according to the Medina classification. By pairwise comparison, the CT bifurcation score showed higher predictive performance for SB occlusion (c-statistic = 0.749) compared with the RESOLVE score (c-statistic = 0.627) or Medina classification (c-statistic = 0.631 to 0.551) (p < 0.05 for all). The CT bifurcation score also consistently improved the reclassification of prediction by the RESOLVE score or Medina classification (categorical NRI = 0.23, continuous NRI = 0.65–0.71, IDI = 0.11–0.14, p < 0.01 for all). The optimal cut-off of the CT bifurcation score was ≥ 1, which showed sensitivity, specificity, PPV, NPV, and accuracy of 90%, 42%, 23%, 96%, and 50%, respectively.
The current study found no relationship between sex and SB occlusion in the studied cases. There were highly significant correlations between CT bifurcation score and age (r = 0.5, p < 0.001). Our results are consistent with Wolny et al. [20] as there were positive moderate significant correlations between CT bifurcation score and age.








