Introduction
Ever since the new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged in December 2019, its clinical manifestation (coronavirus disease 2019 – COVID-19) has been spreading rapidly, resulting in a global pandemic. By April 8 2022, there had been about 496 million confirmed cases, which resulted in at least 6 million fatalities. Some reports correlate more pronounced cardiovascular symptoms with coronavirus infection. They support the hypothesis that patients with pre-existing cardiovascular conditions are more susceptible to a severe case of COVID-19 [1] and, by extension, further damage to the cardiovascular system. Systematic autopsies and percutaneous multiple organ biopsies confirm that COVID-19 patients suffer from multiple organ system dysfunction. External factors (such as government-imposed lockdowns, social distancing and travel restrictions), as well as psychological factors (fear of infection in public spaces and healthcare facilities), played a huge role in decreasing the willingness to reach for medical services. This undoubtedly had an effect on the number and characteristics of cardiovascular disease (CVD) patients admitted to hospitals [2].
At first, the unknown nature of this disease and the initial fear of infection undoubtedly decreased the effectiveness and quality of healthcare. A transformation of institutions and departments to COVID dedicated hospitals can be given as a prime example. Other medical services (including most of the scheduled hospitalizations or consultations) were cancelled or postponed to focus on COVID-19 patients and minimize the risk of further infections [3].
According to the GUS (the Polish Main Statistical Office), the number of deaths in 2020 exceeded the mean value of the last 50 years by over 100 thousand (477 thousand compared to 364 thousand), while the mean number of deaths in a population of 100 thousand reached the highest value since 1951. Among the unexpected deaths in 2020, only 43% were related to SARS-CoV-2 infection, as reported by sanitary stations. However, it must be noted that 27% of those cases had SARS-CoV-2 infection in the past.
As the pandemic continued, the excess mortality in 2021 surpassed the mean value of the last 50 years by over 154 thousand deaths (519.5 thousand compared to 366 thousand), while the death count in a population of 100 thousand reached a value higher than 2020 by about 117 deaths.
According to World Health Organization (WHO) estimates, the number of deaths associated either directly or indirectly with COVID-19 between 1.01.2020 and 31.12.2021 reached 14.9 million. The mortality was significantly higher among patients who were COVID-19 positive [4, 5].
Patients affected by COVID-19 are at increased risk of myocardial infarction, myocarditis, venous thromboembolism, arrhythmias, and exacerbation of heart failure [6]. Severe systemic inflammation increases the risk of atherosclerotic plaque disruption and myocardial infarction. Further, systemic inflammation, abnormal coagulation status, multiorgan dysfunction, and critical illness are all potential contributing factors to the increased risk of thromboembolic events [7]. Studies report remarkable pathway abnormalities in patients with COVID-19, including elevated D-dimer values [8, 9].
Due to the fear of infection alone, more than a half of patients suffering from myocardial infarction chose not to attend the medical care or postponed their admission to hospital, which resulted in a further increase of complication risk [10].
Elective cardiac procedures (such as coronary angiography or percutaneous coronary intervention for stable coronary artery disease) were mostly recommended for deferral by health authorities. For patients developing a myocardial infarction, particularly ST-elevation myocardial infarction (STEMI), emergency reperfusion remained a method of choice and in many cases, a lifesaving procedure. This was reflected in the recommendations of both the Society for Cardiac Angiography and Interventions and the American College of Cardiology. Nevertheless, a significant (40–50%) reduction in the number of myocardial infarction (MI) cases treated in cardiac catheterization laboratories in the year 2020 was observed when compared to 2019. This holds true in regards to both STEMI and non-STEMI patients [5, 10, 11].
Therefore, in the current review we focus on analyzing mortality and morbidity in patients who suffered from acute coronary syndrome (ACS) during the COVID-19 pandemic, as well as investigating the factors that may have a significant impact on their baseline characteristics and outcome.
Number of hospitalizations and time to reach medical care
Twelve studies noted a significantly lower number of admissions for myocardial infarction as compared to the same timeframe in years prior to the pandemic. Furthermore, some of them reported that the number of admitted patients declined by as much as about 50% [4, 12–22]. On the other hand, Marijon et al. observed greater incidence of acute myocardial infarction (AMI) in 2020 than in the years 2012–2019, as well as decreased survival in those cases [3]. Wienbergen et al. did not document a difference in the number of patients treated between 2020 and 2006–2019 per year [2].
Nine studies reported that door-to-balloon time was longer during the pandemic [3–5, 13, 15, 16, 22, 23]. Further, Popovic et al. noted delayed hospital presentation (nearly 25% of patients were admitted to the hospital more than 8 h after the initial symptom onset) [10].
In addition, there are studies that address the aspect of treatment delay in coronavirus positive patients with respect to catheterization lab on- and off-hours [24]. Patients diagnosed with COVID-19 were exposed to longer time from first medical contact to angiography in both cases (on-hours: 133.8 min vs. 117.1 min; p = 0.001; off-hours: 148.1 min vs. 112.2 min; p = 0.003). However, the authors underline that there was no influence of COVID-19 diagnosis on mortality and the prevalence of other periprocedural complications irrespective of time of intervention.
On the other hand, Wienbergen et al. noted that the time interval from symptom onset to interventional treatment of patients was lower in the year 2020 compared with the years before [2].
Some authors report that more acute coronary syndrome patients were admitted in 2020, with a remarkably higher percentage of STEMI cases. However, Perrin et al. did not observe a difference between the number of STEMI during the pandemic period and previous years [23]. In other studies, lower admission of NSTE-ACS patients was observed and the number of STEMI patients remained unchanged [13, 14, 23].
Similarities can be found to previous pandemics and the burden that they presented to the healthcare system. During the Middle East respiratory syndrome (MERS) outbreak, for example, 33% fewer admissions to emergency services were observed (with 14% fewer admissions for MI) [25, 26]. While the reasons for this reduction are difficult to evince, some hypotheses have been made.
Greater reluctance to seek medical care, which might stem from a fear of infection or contagion, is usually the first given theory. Stay-at-home recommendations and global news might have exacerbated the fear, which could have influenced the patients to postpone or cancel urgent procedures. In England, surveys revealed that the fear of being exposed to COVID-19 was the most common reason for the decrease in ACS admissions [20]. Similar healthcare avoidance may explain increases in out-of-hospital cardiac arrests in countries such as Germany, France and Poland. A French study suggested a similar ACS occurrence during the lockdown when compared to pre-COVID periods, even if earlier studies claimed a reduction of CVD early on in the pandemic caused by environmental factors or changes in lifestyle (such as less road traffic and a higher amount of physical exercise [2, 3, 11].
Changes in the healthcare system as a result of the pandemic are usually given as another explanation. Factors that may lead to an overall reduction in admissions include: deferral of less urgent cases, stricter requirements for referral to the healthcare facilities, decreased availability of intensive care units and fewer cardiovascular admissions in outpatient clinics. The first factor may also play a role in the observed difference between the reduction in hospitalizations in STEMI and non-STEMI (NSTEMI) patients, with the former experiencing more severe symptoms. Interestingly, previous research implied that CVD patients experienced much more severe COVID-19 symptoms [20, 27]. A study from the United States supports this claim, by revealing that patients with AMI and COVID-19 were older and had more co-morbidities when compared to patients without COVID-19 [28].
The risk of undiagnosed signs of MI in patients admitted for COVID-19 symptoms may be even higher. The focus of the medical staff is usually shifted towards COVID-19 prevention (e.g. separate registration for patients suspected of infection and other isolative measures), which also can result in fewer admissions for MI [27].
However, some studies prove the efficacy of the local healthcare system. Smith et al. found that the first medical contact (FMC) to balloon time, door-to-balloon time as well as the time to first electrocardiogram (ECG) remained unchanged. As such, departments that successfully aided in triaging and treating STEMI cases allowed the personnel available to handle the patients efficiently, even if the triaging process became more complicated due to the additional infection control protocol [22].
Finally, the social isolation of patients caused by the lockdowns could have led to some MI signs being overseen. An increased risk of early mortality and more pronounced severity of symptoms is much more common in lonely people. They also experience a myriad of mental health issues such as household stress, fear of unemployment, depression and anxiety about the upcoming future. These effects are known CVD risk factors, especially in the elderly population [29, 30]. Atypical symptom presentation in the elderly could also lead to confusion and discouragement from seeking medical care [11]. All of these factors show the increased risk of exacerbating adverse psychological effects of the COVID-19 pandemic in the elderly population [31].
In summary, changes in the number of hospitalizations and changes in the time to reach medical care were noted by almost every investigator who analyzed the process. Those changes were different and mostly dependent on local healthcare accessibility, but in the majority of reports there was a shift towards longer time to reach medical care, lower overall number of admissions and greater percentage of STEMI patients.
Baseline patient characteristics
Patients who underwent percutaneous coronary intervention (PCI) during the coronavirus pandemic were younger than patients from 2019 and were less likely to have diabetes, hypercholesterolemia, hypertension or a previous myocardial infarction [5]. There was, however, an increase in pre-hospital sudden cardiac arrest (SCA) as well as STEMI cases in the year 2020 [3, 11, 14, 20]. On the other hand, three research groups did not find noteworthy differences in mean patient age, gender, medical history of the patients, diabetes mellitus or smoking [2, 12, 16]. Some studies report that a significant reduction in STEMI admissions in female patients was more pronounced than in males during the pandemic [12, 32].
Another three studies concluded that there were no statistically significant differences in baseline characteristics of ACS patients when comparing the pandemic and pre-pandemic periods. However, a higher median peak value of troponins in the ACS population as a whole was observed [13, 14, 23].
The subset of patients suffering from diabetes showed a higher rate of multivessel coronary artery disease diagnosis during the pandemic. In the same study, rates of cardiogenic shock, out of hospital cardiac arrests, and infarct locations remained unchanged [4].
The impact of inadequate control of non-communicable diseases on populational health cannot be avoided. For example, diabetes mellitus (DM) is a huge risk factor for admission to intensive care, invasive ventilation as well as death in COVID-19 patients [33]. Increased COVID-19 severity and mortality have been observed in diabetic patients with higher glycated hemoglobin (HbA1c) and glycemia values [34]. Further, higher HbA1c increases the risk of a poorer outcome in acute coronary syndrome patients – which highlights that stricter glycemic control of diabetes patients is of utmost importance, regardless of the pandemic. This issue was addressed by a report which revealed that more than 100 000 people in the UK missed or delayed their HbA1c testing. The report shows that the societal restrictions imposed during the lockdown negatively affected the outcome of diabetes patients [35].
In the patients with ST-elevation myocardial infarction with COVID-19 infection, elevated levels of biological markers of inflammation (C-reactive protein, fibrinogen, D-dimer) and increased occurrence of antiphospholipid antibodies were noted [10].
The impact of out-of-hospital cardiac arrest (OHCA) in the era of the coronavirus pandemic must be discussed. There are multiple studies that address this matter. In London, as an example of a large city with optimal healthcare accessibility, an 81% increase in OHCA during the pandemic was observed [36]. Further, the authors noted fewer resuscitation attempts (36.4% vs. 39.6%, p = 0.03) and longer emergency service response times (9.3 vs. 7.2 min, p < 0.001). As a consequence, survival at 30 days post-arrest was poorer during the pandemic (4.4% vs. 10.6%, p < 0.001). This might have not only affected baseline characteristics of acute coronary syndrome cases reaching the hospital, but also limited their survival prior to hospital admission. A similar study conducted in the United States noted that the proportion of cases receiving bystander cardiopulmonary resuscitation was lower in 2020 (61% to 51%, respectively; p = 0.02), and bystander use of automated external defibrillators (AEDs) declined (5% to 1%, respectively; p = 0.02). Emergency services response time increased (6.6 ±2.0 min to 7.6 ±3.0 min, respectively; p < 0.001), and fewer OHCA patients survived to hospital discharge (14.7% to 7.9%, respectively; p = 0.02) [37]. In Italy, where the fear of coronavirus was greatly pronounced due to huge mortality at the pandemic onset, there was a reduction in cardiopulmonary resuscitation performed by bystanders (OR = 0.94; p = 0.029) and in the return of spontaneous circulation (OR = 0.621, p < 0.0001), while there was no significant reduction in the use of Public Access Defibrillators [38]. All these studies show that the baseline on admission and final outcome in acute coronary syndrome patients during the pandemic might have been affected by the response prior to reaching medical care.
In general, some reports emphasize that younger and less ill patients were more likely to suffer from acute coronary syndrome. Others did not find such a relation. Notably, higher troponin values on admission, which are reported by most studies, are clearly associated with increased time to reach medical care.
Invasive treatment
Research papers have reported a decrease in the average number of percutaneous coronary interventions for patients undergoing elective procedures [13, 17, 20]. An 18% reduction of PCI was observed in STEMI patients, while for NSTEMI patients this reduction was 37%. For acute coronary syndrome in general, the reduction of angiographies without PCI reached 60%. After the government-imposed lockdown in England in 2020, performance of PCI procedures dropped by 49%, with the highest decrease in elective procedures (66%) as well as NSTEMI/unstable angina indications (45%). A less prominent decline was observed in PCI for STEMI indications (33%). These declining numbers of PCI procedures have been particularly noticeable in the elderly population [20].
Three studies showed no difference in the number of PCI during the outbreak and the period before the pandemic [2, 4, 19]. Interestingly, an increased use of radial access and DES during the pandemic was observed [11].
Compared to 2019, patients who underwent PCI were younger, stayed for a shorter period of time and were discharged home more often [3, 11, 14, 20].
In some studies, thrombolytic treatment was needed more frequently than in the previous years, which was justified by reluctance to carry out primary PCI in patients who had international travel history along with suspicious symptoms of COVID-19 [13]. The number of rescue procedures after failed thrombolysis remained unchanged [11].
The overall number of patients referred for coronary artery bypass grafting (CABG) surgery was relevantly lower. The number of patient referrals for CABG during initial hospitalization remained unchanged, but the number of scheduled surgical procedures, planned after being discharged from the hospital, decreased. In some reports, an 80 percent reduction of CABG was observed, which was correlated with an increase in local incidence of COVID-19 [11, 13, 17, 18, 20, 39].
Essentially, the main conclusion from the literature is that the number of invasive procedures dropped significantly during the pandemic, which was most spectacular in the field of surgical revascularization. Probably, both physicians and patients less frequently continued intended, post-discharge treatment. Further, in patients with less severe multivessel disease, complex and staged percutaneous coronary interventions were performed during the initial hospitalization to a higher degree than during the pre-COVID period. In addition, CABG is usually performed in NSTEMI patients, who were admitted less frequently in 2020. This may explain the lower total number of performed CABG procedures in compared timeframes [40].
As discussed before, the focus of healthcare has been shifted towards aiding COVID-19 patients – which led to a critical reduction of both planned and actually performed surgical interventions. The effect will probably be long-lasting and will have a great impact on society in general (which may be associated not only with increased treatment costs, but also prolonged exclusion of patients with delayed procedures from employment or the healthcare system having less funds to perform its tasks) [18].
The technical debt accumulated in the healthcare system spills over to residents in the surgical area. The surgeons had less practical training due to a lower number of surgical procedures being performed (both elective and emergency). Further, they were often delegated to support the intensive care units and dedicated COVID-19 wards [18].
As Almeida concluded, low-risk patients would benefit from delaying their elective surgical procedures, while high-risk patients were recommended to have their procedures performed as indicated, because a delay could have caused worse outcomes [18]. This effect is visible in all healthcare areas and has been presented by most studies cited by the current report.
Hospitalization outcome
Early diagnosis and proper treatment are of utmost importance for MI and any shortcomings can be fatal in nature. Patients who did not consult a physician immediately after observing the initial symptoms, who were admitted to the healthcare facilities when symptoms became too painful to handle, ended up not eligible for revascularization or with prolonged ischemic time.
All of the infection-containing precautions, such as changing of the protective gear by staff, temperature measurement, chest X-ray and travel history tracking, add to the time needed to perform the treatment. The resulting delay could lead to an increased mortality rate, higher incidence of malignant arrhythmia and cardiogenic shock. As a result, existing myocardial infarction survivors may experience debilitating or even deadly heart failure in the future [15]. Studies reveal that untreated ACS led to multiple acute and long-term complications, such as mitral regurgitation, aneurysmal dilatation, cardiac rupture, and pericardial tamponade, as well as a significant reduction in left ventricle ejection fraction. All of these may cause immediate cardiogenic shock and late chronic heart failure [16].
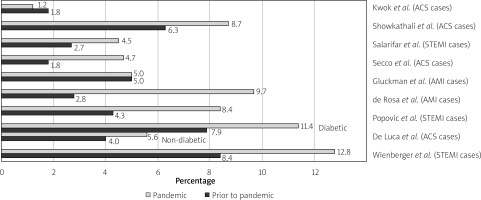
In-hospital mortality was found to be remarkably higher in the year 2020 when compared to time intervals prior to the pandemic [3–5, 16, 21] (Figure 1, Table I). Additionally, multiple studies report a greater number of adverse events [2, 4, 11, 12, 14, 22]. Notably, higher risk calculated with the GRACE score was recorded during the pandemic [3, 5, 14–16]. A study from the United States found that in the year 2020, STEMI patients experienced a 54% higher rate of cardiogenic shock as well as a 29% higher rate of OHCA (out-of-hospital cardiac arrest), with a 52% higher overall hospital mortality rate compared to previous years [2].
Table I
Evaluated studies
| First author | Publication date | Country | Study population | Analyzed parameters | Analyzed time intervals | Major findings |
|---|---|---|---|---|---|---|
| Smith et al. [22] | April, 2021 | United States | 100 MI patients (52 from 2019, 48 from 2020) | STEMI door-to-balloon times | 16/3/2020–31/08/2020 vs. 16/3/2019–31/8/2019 |
|
| Ishii et al. [19] | September, 2020 | Japan | First 367 patients with ACS Second 370 patients Third 375 patients | PCI procedures | 15/4/2020 vs. 30/4/2020 vs. 15/5/2020 | |
| Kwok et al. [20] | November, 2020 | United Kingdom | 126 491 patients | PCI procedures | 1/1/2017–31/12/2019 vs. 1/1/2020–22/3/2020 vs. 23/3/2020–30/4/2020 |
|
| Hawranek et al. [11] | January, 2021 | Poland | 7844 (2019) 3457(2020) | Characteristics and treatment | 1/3/2019–31/5/2019 vs. 1/3/2020–31/5/2020 |
|
| De Rosa et al. [12] | April, 2020 | Italy | 618 (2019) 319 (2020) patients with AMI | Number of hospitalizations, patients with STEMI and NSTEMI | 1 week period during the COVID-19 outbreak, compared with the equivalent week in 2019 |
|
| De Filippo et al. [21] | 2020 | Italy | 547 patients with ACS | Number of hospitalizations, outcomes | 20/2/2019–31/3/2019 vs. 1/1/2020–19/2/2020 | |
| Perrin et al. [23] | December, 2020 | Switzerland | 45 (group of interest) 140 (control group) | Symptom onset to first medical contact, number of hospitalizations, characteristics of patients | 13/3/2020–30/4/2020 vs. 13/3/2019–30/4/2019 and 7/1/2020–24/2/2020 |
|
| De Luca et al. [4] | December, 2020 | Italy | 6609 patients | Symptom onset to first medical contact, number of PCI procedures, characteristics of patients, outcomes | 1/3/2019–30/4/2019 vs. 1/3/2020–30/4/2020 |
|
| Popovic et al. [5] | June, 2020 | France | 83 patients with STEMI during the COVID-19 pandemic vs. 1552 patients between 2017–2018 | Characteristics in patients with COVID-19 who underwent PCI | 2017–2018 vs. pandemic period |
|
| Wienbergen et al. [2] | April, 2021 | Germany | 726 patients with STEMI in 2020 vs. 10226 patients between 2006–2019 | Number of hospitalizations, patient characteristics, treatment | 2006–2019 vs. 2020 |
|
| Showkathali et al. [13] | September, 2020 | India | 104 patients with ACS in 2020 vs. 183 in 2018–2019 | Number of hospitalizations, patient characteristics, treatment, outcomes | 2018–2019 vs. 25/3/2020–31/5/2020 |
|
| Gluckman et al. [14] | August, 2020 | United States | 15244 patients | Number of hospitalizations, patient characteristics, treatment, outcomes | 30/12/2018–22/2/2020 vs. 23/2/2020–28/3/2020 vs. 29/3/2020–16/5/2020 |
|
| Tam et al. [15] | April, 2020 | China | 149 | Number of hospitalizations | 1/11/2019–24/1/2020 vs. 25/1/2020–31/3/2020 | |
| Secco et al. [16] | April, 2020 | Italy | 162 patients in 2019 (March) vs 84 patients in 2020 (March) with ACS | Number of hospitalizations, patient characteristics | 3/2019 vs. 3/2020 |
|
| Mafham et al. [17] | July, 2020 | United Kingdom | 3017 patients in 2019 vs. 1813 in 2020 | Number of hospitalizations | 2019 vs. 2020 | |
| Marijon et al. [3] | May, 2020 | France | 521 vs. 3052 | Number of hospitalizations, outcomes | 16/3/2020–26/4/2020 vs. 12–17 weeks in 2012–2019 |
|
| Huang et al. [43] | January, 2022 | China | 1138 patients, 552 after both the vaccine vs. 586 control groups | Association between non-mRNA COVID-19 vaccine and outcomes in acute coronary syndrome cases |
| |
| Case et al. [52] | January, 2022 | United States | 5217 patients who received the COVID-19 vaccine | Trends of hospital encounters for vaccine recipients before and after vaccination | 10/12/2020–13/8/2021 | |
| Garcia et al. [46] | April, 2022 | United States | 586 patients, 227 in 2020, 359 in 2021 | Trends of COVID-19 positive patients with STEMI during the course of the pandemic | 01/2020–12/2020 vs. 01/2021–12/2021 |
|
| Holman et al. [34] | August, 2020 | United Kingdom | 264390 people with type 1 diabetes 2874020 people with type 2 diabetes | Mortality in people with type 1 and type 2 diabetes during the initial COVID-19 pandemic | The first 19 weeks of 2020 vs. 2017–2019 |
|
| Sheikh et al. [49] | February, 2022 | Pakistan | 4480 patients, 1216 March–July 2019, 806 March–July 2020, 1304 August 2019-January 2020, 1157 August 2020-January 2021 | Number of hospitalizations | 03/2019–07/2019 vs. 03/2020–07/2020 vs. 08/2019–01/2020 vs. 08/2020–01/2021 |
|
| Mafham et al. [17] | August, 2020 | United Kingdom | 3017 patients in 2019, 1813 patients in 2020 | Number of hospitalizations and procedures, outcomes | 01/2019–05/2020 |
|
| Legutko et al. [39] | May, 2020 | Poland | 1898 coronary angiographies, 1608 percutaneous interventions | Number of coronary angiographies and percutaneous coronary intervention procedures | 1/1/2020–14/5/2020 | |
| Salarifar et al. [32] | December, 2020 | Iran | 324 patients | Patient outcomes at a median time of 70 days during the pandemic | 29/2/2020–30/04/2020 vs. 01/03/2019–30/04/2019 | |
| Quesada et al. [48] | May, 2022 | United States | 585 STEMI patients with COVID infection | Mortality | 1/3/2020–31/12/2021 | |
| Case et al. [52] | April, 2021 | United States | 1533 patients admitted with myocardial infarction | Mortality in COVID vs. non-COVID patients | 1/3/2020–30/6/2020 |
|
| Fothergill et al. [36] | March, 2021 | United Kingdom | 3122 patients in cardiac arrest during the pandemic, compared with 1724 patients prior to pandemic | Incidence of OHCA, mortality, first aid in OHCA | 1/3/2020–30/04/2020 vs. 1/3/2019–30/04/2019 |
|
| Uy-Evanado et al. [37] | January, 2021 | United States | 231 out-of-hospital cardiac arrest cases in 2019 and 278 cases in 2020 | Community response to out-of-hospital cardiac arrest | 1/3/2020–31/5/2020 vs. 1/3/2019–31/5/2019 |
|
| Stirparo et al. [38] | October, 2022 | Italy | 12140 out-of-hospital cardiac arrests in 2019 vs 13372 cases in 2020 | Cardiac arrest occurrence, when CPR started and whether the bystanders used public access to defibrillation | 1/1/2020–31/12/2020 vs. 1/1/2019–31/12/2019 |
|
| Tokarek et al. [24] | August, 2021 | Poland | 11348 patients with ST-segment elevation myocardial infarction | Treatment delay and clinical outcomes in COVID-19 positive and negative patients with ST-segment elevation myocardial infarction (STEMI) | 1/3/2020–31/12/2020 |
|
There were two studies, however, which showed no difference in in-hospital mortality (IHM) between the years 2020 and 2019 [13, 17]. Similarly, Kwok et al. established that there was no significant change in in-hospital outcomes (such as mortality and peri-procedural complication rates) when comparing pre-COVID-19 and COVID-19 pandemic periods [20]. Notably, those results reflect the overall cohort of patients, including stable coronary artery disease cases.
The mortality rate of the COVID-19 patients was noticeably higher [4]. Similarly, major adverse cardiac events were found to be more prevalent among patients with the COVID-19 infection [22]. Further, myocardial infarction with concomitant COVID-19 was associated with increased in-hospital mortality [30]. On the other hand, Weinbergen et al. found no correlation between COVID-19 infection and the effect of cardiac treatment [2].
Studies showed that the length of hospital stay was longer in COVID-19 patients [13]. Other researchers noted that hospitalizations during the pandemic were shorter in general [14, 17, 20]. Shorter hospitalization and more frequent home discharge for PCI patients should be emphasized. The reasons include the already mentioned reluctance of older patients to be admitted to the hospital, patients themselves preferring to be discharged earlier, their fear of contracting SARS-CoV-2 in the hospital after the medical procedure, as well as efforts by the institutions to provide readily available hospital beds [14].
Almeida et al. report that longer timespans between the positive reverse transcription polymerase chain reaction (RT-PCR) for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the time of surgery resulted on average in better outcomes of the medical procedures [18].
In summary, nearly all research papers report a higher number of adverse events and greater mortality during the COVID-19 pandemic. This was valid for both patients with and without coronavirus infection.
Worldwide differences in evaluated parameters
As mentioned before, there were some divergences regarding acute myocardial infarction hospitalizations and their outcome in accordance to geographical region. An interesting meta-analysis was conducted by Sofi et al. [41]. They included 111 557 STEMI cases from 57 countries during the coronavirus pandemic. The authors calculated that around 20% reduction in STEMI hospitalizations was reported for Europe (RR = 0.81; p < 0.0001), Asia-Pacific and Middle East (RR = 0.83; p < 0.0001), and the North, Central, and South America (NCSA) region (RR = 0.76; p < 0.0001). Latin America countries reported the largest decrease in STEMI hospitalizations (> 50%), whereas France, Denmark, and South-East Asia reported no appreciable decrease. Further, the authors note that STEMI hospitalizations decreased in countries with lower hospital bed availability, whereas they stayed around historical levels in countries with much greater bed availability, suggesting that hospital beds had been overwhelmed with COVID-19 patients. This hypothesis was supported by Sorci et al., who underline the role of comorbidities and socio-economic and political factors as potential drivers affecting how a country deals with globally threatening epidemics [42]. Of note, the authors report the highest COVID-19 case fatality rates in France, Belgium and the United Kingdom and the lowest in Bahrain, Sweden and South Korea.
Changes after vaccine rollout
The invention and subsequent deployment of vaccines against COVID-19 had a significant effect on lowering morbidity and subsequent mortality caused by the disease – in effect slowing down the pandemic [43]. The first SARS-CoV-2 vaccine authorized for medical use in December 2020 was the BNT162b2 mRNA vaccine (made jointly by Pfizer and BioNTech) [44, 45].
As an effect of the availability of newly developed vaccines, alterations in baseline patients’ characteristics could be observed. Patients admitted to hospitals in 2021 had a higher chance of being Caucasian, having chest pain instead of dyspnea and their chances of having pre-PCI shock or infiltrates on chest X-ray were lower when compared to 2020 [46].
As regards medical procedures, there has been an increase in the use of invasive angiography (86% in 2021 vs. 77% in 2020). There was no noticeable difference in the frequency of PCI (primary and rescue PCI combined) between 2021 and 2020 – this procedure remained the primary revascularization method, used in more than 70% of cases. For primary PCI patients, the door-to-balloon time changed from 50–122 min (2020) to 50–106 min (2021), among which the percentage of patients having a door-to-balloon time of under 90 min was 59% and 64%, respectively. Cases where optimal medical therapy was sufficient increased from 19% (2020) to 25% (2021). Coronary artery bypass grafting surgery and thrombolytics were rarely used [46].
The length of hospitalization decreased from 3–15 days to 2–12 days; duration of stays in intensive care units underwent a similar reduction – 1–6 days in 2021 compared to 1–11 days in 2020 [46]. Based on a multivariate analysis of complete data, the risk of in-hospital mortality in 2021 was found to be 25% lower when compared to 2020 [46].
Other studies found that respiratory symptoms and pathology on chest X-ray were less frequently observed in vaccinated patients. In-hospital deaths were noted more frequently for unvaccinated patients. In this cohort, time between vaccination and STEMI was found to be 20 days [46–48].
According to Huang et al., patients who were vaccinated had a lower risk of cardiac readmission [43].
A study from Pakistan found that there were 11.2% fewer ACS hospitalizations in the year 2021 when compared to analogous months in the year 2020, while patient presentation remained largely unchanged between the two periods [49].
Those results need to be confronted with potential cardiovascular complications of vaccination. The incidence of cardiac outcomes after mRNA COVID-19 vaccination was highest for males aged 12–17 years after the second vaccine dose; however, within this demographic group, the risk for cardiac outcomes was 1.8–5.6 times as high after SARS-CoV-2 infection than after the second vaccine dose. As such, the benefits of COVID-19 vaccines outweigh the potential risks of adverse events [50].
In general, vaccinations against COVID-19 have proven to be effective and safe in COVID-19 prevention, limiting disease severity, hospitalizations and mortality rates [51], but they also altered the procedures and improved healthcare efficacy.
Challenges in the near future
There are still challenges which may await society in the near future – such as significant vaccination hesitancy in some countries or the emergence of new and unpredictable strains of the virus (such as the Delta, Delta-plus, Omicron and Lambda strains). Furthermore, the factors responsible for the COVID-19 complications will still be present in potential future waves of this or other infectious diseases. This calls for the healthcare system to establish standard operating procedures and policies to ensure proper and efficient care for ACS patients under similar conditions. The advances in telemedicine during the pandemic allowed the quality of the healthcare to be improved [51].
Wearing full personal protective equipment during primary percutaneous coronary intervention and proper protection in the catheterization lab for STEMI patients with a confirmed or suspected COVID-19 infection have been adopted as standard operating procedures. There is a need for increased messaging to educate society on the importance of seeking immediate medical care in the case of acute cardiac symptoms as well as incentivizing COVID-19 vaccination. Vaccination was shown to be both the safest and most successful method to counteract the pandemic [44, 51, 52].
Conclusions
As a conclusion of this review, we emphasize that the pandemic had a great impact on overall populational mortality and morbidity, which was greatly pronounced in patients with cardiovascular disease, particularly in acute coronary syndrome cases. The patients who suffered from ACS differed in baseline characteristics, they underwent different treatment and their outcome was worse as compared with the period prior to the pandemic.